
Gigi Farrell
When the Blood Drives Were Canceled
Gigi Farrell Registered nurse and department manager of Nursing and Community Wellness at San Diego Blood Bank
As told to Erin Meanley Glenny
I manage San Diego Blood Bank’s main donor center near downtown and the one in El Cajon. I’ve been with the organization for 20 years and thought I had seen it all until COVID-19.
We supply blood to nearly 50 hospitals in the region; including some hospitals in Orange and Los Angeles counties such as City of Hope.
We usually have a general sense of what each hospital will use each week. We have real-time eyes on hospital supply and can see when there is a major drop, perhaps due to an emergency. This is why it is so important to have a 5-to-7-day supply on hand. At times during the pandemic, we’ve had less than a half-day supply of several blood types for several days in a row.
Each month, we typically collect about 2,800 pints of blood at our six centers and more than 5,000 pints from our bloodmobiles. So more than 60 percent of the local blood supply is collected on our bloodmobiles. We normally have six to 10 of them out in the community on any given day.
Around mid-March, our bloodmobile drives began to cancel due to schools closing and companies switching to remote work. We didn’t have enough blood on the shelves, and it was scary. We immediately jumped into sending out the plea—everyone was tweeting. We asked younger donors to step up to allow older donors to stay safe at home. The community answered our call, like they always do.
People were waiting two hours. It got very overwhelming. There was a point when we had an eight-day supply—that was unheard of.
Over my 20 years working at the blood bank, I have found that tragedies bring donors in—I was at SDBB in the days after 9/11. We had donors in lines around the building, waiting hours to donate. I believe people need to be with the community so we can mourn together and support one another. Coronavirus is slightly different, in the sense that there’s so much fear of the unknown out there.
Because a lot of our donors are baby boomers, we really need to bring the younger generation in, the millennials, Generation X. We got a lot of new donors, first-timers coming in, but we need them to come back. It’s not a one-time thing. The blood is only good for 42 days, and it is usually out the door within a few days. The platelets, in the blood plasma, have to be used within five days.
We need more COVID-19 convalescent plasma (CCP), which we collect from donors who have recovered from the illness. One CCP donation can help as many as three or four patients still fighting COVID-19. The demand for convalescent plasma in June was double that of May, and as of July we are starting to see even higher demand—we need more recovered patients to sign up.
Many hospitals have told us that our ability to stand up our CCP program so quickly was almost unheard of.
On a personal note, I reached my 15-gallon milestone recently, and donated in honor of my Uncle Rudy, a regular blood donor who was admitted to the hospital in April for a critical case of pancreatitis. Rudy received eight pints of blood over the course of five surgeries. These units saved his life, and it really hit home for me and reminded me of my purpose.

Dr. Wilma Wooten
Dr. Wilma Wooten
San Diego County Public Health Officer
What don’t people seem to be understanding right now?
That we all have the power for personal and collective action—and we should use it. The pandemic is not over by any stretch. The virus is still here, and it’s likely to be with us for a while longer. We can’t be complacent and go back to living our pre-COVID lives. We all play a role. The health, and in some cases, life of someone’s child, parent, grandparent, or loved one is at stake. Wearing a face covering, maintaining physical distance from those not in your household, washing your hands frequently, and avoiding gatherings are small steps that can have a big collective impact.
What’s your greatest challenge right now?
Personally, a challenge I share with public health officials worldwide is not internalizing attacks on my character. I fully understand and appreciate that this is an inordinately stressful time and sympathize with the frustration, hardship, and other complicated feelings around this pandemic’s impact on our lives. Every once in a while, an attack is so personal and so off-base that it can feel unfair, but I take a breath and remind myself that this person is likely struggling and all my actions need to be focused on helping everyone cope with today and prepare for tomorrow.

Elvin Lai
Elvin Lai
Fourth-generation hotelier, Ocean Park Inn
How long did you have to close the hotel this spring? How did you adapt the business?
We closed the hotel for two months. Since we were already in renovation mode before COVID-19, we took the opportunity to move some projects up on the schedule for completion. Adapting to COVID-19 protocols for our guests wasn’t much of a leap. We faced the hepatitis A outbreak just prior and the industry—and we, as independent operators—mobilized to keep our staff and guests safe at that time. That being said, COVID-19 is very different.
Being a small hotel was much more beneficial. We have been able to be more nimble and ready to move fast on the implementation of protocols. But it has been more challenging to source the right materials due to the lack of purchasing power and the lack of a purchasing entity doing it for us. In the end, we found ways to buy directly from out of the country or leaned in hard on our relationships to make plans come through.
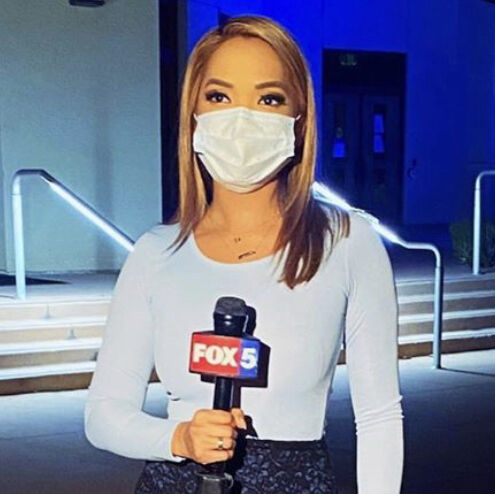
Liberty Zabala
Liberty Zabala
Reporter, Fox 5
How has the nature of your job changed?
We’ve had to adapt to this like everyone else, by taking advantage of technology (conducting virtual interviews) and modifying our equipment (using longer stick mics) to maintain six feet of physical distance. We wear masks, disinfect constantly, and have limited the number of people inside the newsroom to a skeleton crew.

Steven Dinkin
Steven Dinkin
President, National Conflict Resolution Center
With the protests going on, we have to ask, does conflict resolution work in large groups?
The underlying concepts between one-on-one conflict resolution and peaceful large group protesting are essentially the same. Will yelling and screaming or violently protesting help an individual or group be heard, or is it just noise and a distraction? Perhaps a more thoughtful, strategic approach might actually get you closer to the finish line.

Shannon Cotton
From the Front Lines
Shannon Cotton ICU nurse at UC San Diego Medical Center, Hillcrest
As told to Marie Tutko
I work at A COVID-designated ICU. When COVID-19 first came to the US—to San Diego specifically—it was people disembarking from flights at the air bases, and they would send them to the hospital. There were military guards and extreme precautions. Now, we still have patients in the ICU, but it’s much thicker than in the beginning. We’re getting patients from all over Southern California. It’s really busy—the patients are extremely sick and require a lot of nursing care. Nurses continue to show up to work every day, for their patients and community, but we have to stay healthy to take care of people.
It’s really hard to see patients through the glass door. Because of the isolation, we have to keep the door shut and watch them. Maybe they’re confused, or are trying to take out their breathing tube, and you have to make that choice: Do I go in without it, stop the patient from doing this, and risk my own health? Or do I put on my PPE* as quickly as I can and pray that I get there in time? It’s a hard choice that we make every day.
Nurses in my ICU were the first ones who asked for, and practiced, universal masking. We wanted to wear surgical masks through the nurses’ station and every single patient room, whether or not they had tested positive. Nurses really led the fight on this. We continued to do it, despite threats of discipline and even discharge from administration. And now we have a universal masking policy.
We are mostly getting patients from Imperial County, where the positive testing rate—last time I checked—was 23 percent. Some of the sickest patients go to UCSD La Jolla to our COVID ICU, where they get ECMO treatment—extracorporeal membrane oxygenation—in which they move the blood out of your body, reoxygenate it, and send it back into your body through a large catheter. The patient is still intubated with a breathing tube, and ventilated.
I was at work on Monday, and the ICU was nearly at capacity when I left that night. It feels—just the heightened level of adrenaline you walk into the unit with—it feels like everyone is sick and needs you. I assume the hospital is not at capacity since we’re still doing elective procedures and surgeries, but as a front-line worker I rely on hospital administrators to monitor that situation and let us know what’s going on with transparent communication to all staff from their bird’s-eye view. Because to me, it feels like we’re on the verge of a surge, and that we need to start preparing our second ICU to take positive COVID-19 patients. The feeling in the unit is that it could come at any minute.
We worry about our patients when we go home. I’m still thinking about the patient I took care of in that room—did they make it through the night? There is that heightened sense of anxiety, at all times. The nursing staff used to be able to have lunch together at a break, talk about our lives, our kids… now it’s a social-distance-mandated break, and you don’t even have that connection with your coworkers. A lot of front-line staff are going through this emotional toll: I want to show up for my patients every day, and I do. But at what point do I have to take a step back and say, “I need a break for my own family or my own mental health”? It can be exhausting. But we show up every day, and/ we just go.
What’s difficult with really sick patients diagnosed with COVID-19 is that our visitor policy is severely restricted, and there’s very few exceptions. I had a Zoom meeting with one of my really sick patients and four of his family members; it’s hard, because they can’t touch him. They can see him, but it’s not the same as being there and being able to hold their hand. The nurse really does become the emotional support for the patient, and the patient’s only contact at the bedside. In my head, I understand and support the restricted visitor policy. But in my heart, I feel that someone has to be there to help you know that we’re watching you, that we love you. That you’re not just a number. We all try to provide that support to our patients, now more than ever.
We all remember the patients who died from COVID-19. Their families are so grateful for the care. It’s heartbreaking, but we know we did our best, and we fought for their lives as hard as we could. We know who they were. We know their names.
One patient who really sticks in my heart was on the step-down unit. He was requiring more and more oxygen. The nurse on his unit was really concerned, and the doctors brought him to the ICU. When he arrived, the doctors and I had a serious conversation with him: “Your numbers aren’t good and you’re breathing really fast. We have to put in a breathing tube.”
He said, “I have to call my mom.”
My colleague got on his phone and FaceTimed his mother and sister so he was able to tell them, “I’m sick and I’m in the hospital. I probably won’t be able to talk to you for a while, but I’m going to get through this.”
It was amazing to give him that chance to talk to his family, because you don’t know if you’re going to come out on the other side alive or dead. It’s so unpredictable. Within 30 minutes of him transferring to the ICU and making this phone call, we had him on a ventilator—but he eventually recovered, and was discharged home. He holds a special place in my heart.
It’s great to see someone move out of the ICU. In my unit, we clap and cheer when someone recovers and is wheeled out to the step-down unit. A special chime is played when a COVID patient moves out of the ICU or is discharged from the hospital. Everyone knows something good is happening, because usually those overhead announcements are emergencies. But these special chimes—you look up and you wonder if that’s someone you know. It feels like a victory.
*Our PPE is an N95 respirator, a gown, gloves, and a face shield. The hospital doesn’t require shoe coverings or hair coverings, but most of the nurses on my unit use them, simply because this is a novel virus. We just want total protection.

Nancy Maldonado
Nancy Maldonado
CEO, Chicano Federation
What is your biggest fear for San Diego’s Latino community right now?
We don’t have to look further than the COVID-19 infection rate among San Diego Latinos to know this pandemic has exposed and exacerbated inequities that have existed for far too long. Our community’s greatest challenge right now is ensuring that we answer this call to action so that someday, we may be able to look back and see how this terrible moment in time pushed us to finally address structural inequities that make some communities more susceptible to poverty, disease, and death than others. My biggest fear is that we return to “normal” and miss our opportunity to interrupt the status quo and evolve in ways that can lead to a more equitable future.
Sumit Chanda PhD
Hunting for Coronavirus Treatments
Sumit Chanda PhD Professor and director, Immunity and Pathogenesis Program at Sanford Burnham Prebys Medical Discovery Institute
As told to Josh Baxt
For a virologist, when a new influenza or coronavirus comes on the scene, it’s just bad news. In contrast to something like Ebola, where you need close contact with bodily fluids, or Zika, where you need a mosquito to transmit it, these respiratory viruses just need one infected person on an airplane.
We knew from experience that coronaviruses could be dangerous: SARS in 2003, MERS in 2012. But no one had ever worked on this coronavirus—SARS-CoV-2—before, because it didn’t exist; we had to figure out how to grow it, how to manipulate it.
These are skillsets that scientists acquire over years. Because we already had those skills, we went from discovering the virus in January to having a screen done by April. If we hadn’t already done the work in influenza and dengue, there’s no way we could have moved so quickly.
We had a variety of tools we’d developed over the years for other viruses that we could adapt to the coronavirus. We didn’t have to build a biosafety level 3 facility in January. That already existed. If we were forced to start from scratch, we’d still be scratching our heads, going: “How do we get this virus to grow in the lab?”
The investments the government and Sanford Burnham Prebys have made in these programs around flu, SARS, and MERS have helped us, and everyone else around the world, move quickly, both in the therapeutic space and the vaccine space. If no prior investments had been made, we’re talking years, if not decades, to do something comparable.
Looking for COVID-19 Treatments
Working with collaborators in San Diego, Kansas, New York, Hong Kong, and elsewhere, the Chanda lab has used SBP’s high-throughput drug screening capabilities (by which scientists can quickly investigate thousands of potential treatments) to identify existing drugs that might work against the coronavirus.
There are only a certain number of labs that can conduct high-throughput drug screening and work with nasty viruses. We have access to a collection of compounds from Scripps Research and, through collaborators in Hong Kong, we had early access to the virus.
We initially tested around 12,000 compounds and found 30 potential candidates, which are now being investigated further. For companies that had antivirals they thought might work against it, we screened those as well. Given our skillsets and resources, we felt it was our obligation to global health to move as quickly as possible.
Thinking Long Term
In May, the Chanda lab received a $10.2 million Department of Defense grant to develop broad-spectrum antiviral therapies—a grant he initially applied for in June 2019, long before the coronavirus hit.
People need to start viewing pathogens, like SARS-CoV2, as existential threats to our health, to our economy, to civilization as we know it. We’ve been saying this as virologists for a long time, and people said, “This is science fiction, it’s the movies, it’s fear mongering.” We didn’t dodge the bullet this time, and I would say the bullet still just grazed us. I think we need to prepare for a much worse scenario.
We feel the best way to combat this threat is to develop broad-spectrum antiviral drugs. The whole premise of the grant is to move away from the “one bug, one drug” paradigm and develop drug candidates that are effective against multiple respiratory viruses—a broad-spectrum approach, which is commonly used to treat bacterial infections.
We can do that with bacteria because their genomes are so big, thousands of genes, and we can target one mechanism that many bacteria use because we have so many choices. Viruses, by contrast, are super compact. Most have just 20 genes, and there are almost no opportunities to find something that works on a broad swath of viruses.
Our strategy is to target the host—in other words, the people being infected rather than the virus infecting them. Our lab focuses on identifying and understanding the specific proteins in our bodies that viruses hijack to help them grow. If we do these kinds of analyses for enough viruses, we can find hijacking mechanisms common between viruses that we can target therapeutically.
If we can develop these broad-spectrum antivirals, we could have them stockpiled and ready. Then if there was a new, emerging virus, we could send them to the source and completely block the worldwide spread. We put out the fire while it’s still in the ashtray, not when it’s consuming the entire house.

Paul VerHoeve
Paul VerHoeve
CEO, Mission Healthcare
What has been most challenging at work?
We recently had a COVID-19 positive patient on our hospice services in a private home. When building a care plan for a patient at the end of his or her life, we normally would have the family be very involved. However, COVID-19 creates a difficult situation that we haven’t previously faced. From top to bottom, we seem to be learning on a daily basis how to stay safe while also being on the front line caring for people who contract the virus.

Drew Koehler
Drew Koehler
Lifeguard II, City of San Diego Fire-Rescue Lifeguard Division
How is your job different?
When it comes to medical aids we definitely have to take a step back and think about things, ask the right questions before we try to help someone. It’s our duty to make water rescues and perform coastal cliff rescues, but it definitely makes you evaluate safer ways to get things done. We have to remember to keep ourselves up to date with department policies so that we are doing the best possible job at keeping each other safe.
What’s your biggest challenge right now?
Dealing with the large numbers of people on the beach while still maintaining social distance guidelines. Ever since the beaches opened up again the crowds have been massive. It’s been a challenge to still provide the best possible service to the public while keeping our distance, especially when the beaches are as crowded as ever.

Julie Rais Ellis and daughter, Kaia
The Masks Saved the Business
Julie Rais Ellis Owner of Rais Case
As told to Sarah Pfledderer
At the beginning of the pandemic, I planted a handful of sunflower seeds at our brick and mortar. It was the day we officially closed, March 16. It’s incredible to watch a seed sprout and turn into a flower, a reminder that we are a part of nature and a cycle. Rais Case is part of a cycle, too—a garden of its own.
We jumped into 2020 with a business plan to promote our new storefront, The Rising Co., and expand our bag line. One hundred percent of our sales came from our bags and accessories. Then in mid-March we had to stop and temporarily change course.
It all started when one of our team members, Avery, spoke with a nurse friend whose hospital was almost out of masks. Avery shared with me: “It would be amazing if we made masks. Maybe we work directly with her hospital and donate them?”
Honestly, I cannot recall wearing a face mask before then. I was overcome with the feeling that we should sew masks, and stayed up well into the night creating prototypes to share with my team. We began by sewing ourselves, driven by the immediate need for essential workers.
It was all-consuming for the first 60 days, working days, nights, and weekends to meet demands. We created a sewing collective. I had to calculate how to source, produce, distribute, and finance making masks with the resources I had in place. We transitioned my garage into our headquarters, creating a shipping station, inventory storage areas, a workshop space with a cutting surface, sewing stations, and other spaces.
Working alone, we couldn’t keep up, and eventually reached out to our handbag production partners. Because we use local manufacturers, we could train our cut-and-sew team in person, get them materials, and get them up and running making eco-cotton twill face masks immediately.
Making masks has carried Rais Case through the past few months. It kept the lights on and allowed us to keep our team together. We have made approximately 10,000 face coverings to date, and customer purchases directly support our ongoing efforts to donate masks to medical staff and other essential workers across the US.
Now, bags and accessories represent 40 percent of our sales, masks and bandanas 60 percent. We feel blessed to have successfully introduced these new products while helping our community stay safe.
Our most important job as human beings is to grow and nurture those around us. Those sunflowers are in bloom right now at the shop, reminding me that we are a part of that natural cycle.

Dr. Nathian Shae Rodriguez
Dr. Nathian Shae Rodriguez
Assistant professor of Digital Media, San Diego State University
How has the pandemic affected your job?
When everything closed down physically, the university administration basically said, “Get out, you can’t go back.” You needed permission from the deans to come onto campus. Everything was done in haste.
My students were feeling mentally and emotionally drained. A lot didn’t come to class. They were scared. They had to find ways to support themselves; many had lost their jobs. It’s not just teaching, it’s helping support them—finding resources for them, giving them information.
What is one good thing that has come out of this?
The intersectionality issues brought to light from the Black Lives Matter movement. We’re going into the fall being more aware of intersectional oppressions, and more cognizant of our students’ experiences.

Danny Khairo
Jenny Siegwart
Into Overdrive
Danny Khairo Co-owner of Alta Dena Drive Thru Market, Clairemont Liquor, and Anchor Liquor
As told to Erin Meanley Glenny
The Alta Dena Drive Thru Market was already an established drive-thru when my family bought it, but it was just a dairy—milk products, cheeses. It’s been there for 71 years. The guy who started it is the landlord; he’s 97.
My dad and my brother and I have owned the drive-thru for 16 years. Sometimes people call and ask for the old Alta Dena ice cream, where it was a powder and you’d do the mixing. I hardly have anybody ask for it, so it’s not worth it to stock.
We expanded the market to alcohol, snacks, soft drinks, a little bit of everything. Apple juice, firewood. We still carry dairy products. You always get people driving through for the first time saying, “This is so cool, wow. How have we never heard of this?” There aren’t other drive-thrus in San Diego because they don’t give the license out; ours is grandfathered in. You can do a drive-thru with a window, like Burger King, but you can’t drive through the building. A lot of mothers like it because they don’t have to get the kids out of the car seats.
At the beginning of the pandemic, milk sales jumped really high. Milk and eggs were the two hot sellers. I’d say 75 percent more milk, so about 100 to 150 gallons a week.
We’ve always carried toilet paper. Whatever we got our hands on, it would sell out immediately. One person came in and bought everything, 15 four-packs of toilet paper, and it was unfair for the rest. So we limited it to one per person.
Business was a lot better. Because of no bars being open and grocery stores closing early, people realized they could save money here. People didn’t have much to do, and collecting an extra $600 a week did good for us. The grocery stores were always packed, so people were coming to us. The line could be 10 cars deep.
People were afraid to get out of their cars. We wear masks for our own safety. We use sanitizer after every customer.
My brother, my dad, and I worked 13, 14 hours every day. My dad is 62. My brother is 30. We have six employees, not including us, between all three stores. Business was good but really exhausting.

Martha Gilmer
Martha Gilmer
CEO, San Diego Symphony
What new innovations do you think the symphony will keep after everything has reopened for good?
What I love about all of the content we are producing [Symphony Stream virtual performances, podcasts, weekly Lunch & Listen episodes on YouTube] is that it brings the audience closer to our musicians, to music director Rafael Payare, and to each other. The storytelling nature of these productions is something we have talked about for years, and before now had not found a format that worked. The fact that suddenly we all have become adept at using technology to connect makes this communication possible, and I think it will be with us even after we can begin live concerts again. However, the crucial core of the experience remains live performance, and we cannot wait to return to hearing our musicians making music together on our stages with a full audience.

Zara Irshad
Jenny Siegwart
A Little Help From Her Peers
Zara Irshad UC San Diego sophomore
As told to Erin Meanley Glenny
Around mid-March I heard a lot of rumors about the school shutting down, and we kept getting these updates but no one knew what was going on. One by one, classes went online, and then people went on spring break and left all their stuff in the dorm. I had three roommates; one left early and didn’t take her stuff. Her dad came two weeks later to clear out her room.
They kept changing the day when you had to leave. There was a window that kept getting smaller. We had only a few days’ notice. It was overwhelming, stressful, and scary having to leave your friends and not know how long it would be. Everyone was crying. My friends and I had decided to go to Disneyland the weekend before, and we are so glad we did that together.
My parents moved me and my second roommate out at the same time. She stayed with my family for about a week at our house in Rancho Peñasquitos. Then her dad drove down from the Bay Area, but some of her stuff is still in our garage.
It was finals week when we moved out, so the last week of March we had to take our finals online. Professors didn’t have time to construct online plans, and it was very experimental for everyone. That was a challenge—studying for finals in the midst of moving out.
I was taking intermediate Spanish all year; a large part of that is conversation, and it was really hard to facilitate online through Zoom. The teacher did a good job trying to adjust, but I had a lot of frustration because we would be put into Zoom breakout rooms where it’s you and a couple peers on screen with no professor to moderate. I wasn’t getting much out of the conversation.
I was struggling in Spanish and seeing my friends struggle. I was like, I need help. I got an email from the UCSD Communication Department about this mobile app, PEERS edu, that was developed through Connect (a startup accelerator founded at UCSD). I downloaded it and tried it for Spanish. You can have a conversation with a native speaker. My tutor was someone in Spain. You type in what subject you like, it tells you where they’re from and how much they charge. The app uses credits, and the tutor decides the price. You can tutor, be a student, or do both—“earn or learn.”
I thought it really helped, thought it was a cool concept and my friends would benefit from it. The founder, Andres Abeyta, has been working on the concept for four years; I spoke to him and started interning for the company. His goal is to roll it out for college students around California who are trying to adjust.
I’ve learned to be more accountable to myself. It’s very difficult to focus from home—you’re not at a desk in the library. I had to block out times of the day to study each subject. It’s hard not to become discouraged when you’re unable to leave.
I’m excited to see how the school rethinks and restructures, and I’m looking forward to the fall. I wasn’t planning on living on campus for my second year anyway—my plan was always to commute from my parents’ house, but now I won’t have to. I’m hoping to be able to go to my newspaper offices a few times. I recently got promoted to opinion section editor at The UCSD Guardian, so I’m hoping to meet the other editors and writers in person.
Now I appreciate what I had. I look at pictures and wish that was still happening. I was personally so caught up in being busy: going home on the weekends to see my parents, work at a coffee shop, plan things with friends, go to class. I took that chaos as stress. It was really crazy, but honestly, I kind of miss that now.

Paul Downey
Paul Downey
President and CEO, Serving Seniors
How has your job changed since the pandemic started?
I am busier than ever and have become a Zoom master! Serving Seniors had to completely reimagine our operating model—akin to building an airplane in-flight. In February, we served 60,000 meals to low-income seniors. We served over 220,000 meals in June. Pre-pandemic, about two-thirds of our meals were served in 15 senior centers throughout the county. Now, almost all are home delivered. We continue to serve homeless seniors “to-go” meals from our Gary and Mary West Senior Wellness Center downtown every day. We also have had to implement an array of safety protocols to ensure the health of our seniors, staff, and volunteers. I’m proud to say we’ve adapted to the new normal and are meeting our mission to help seniors in poverty.
What worries you the most right now?
PARTNER CONTENT
I worry that we have lost our way as a nation. It boggles my mind that we are divided over a basic human right that everyone is equal and should be treated accordingly. Why is wearing a mask to protect yourself and others from a deadly virus a polarizing political issue? Unless we regain our moral compass—including decency, compassion, and empathy for others—we can’t begin to solve our problems and heal our wounds.


















